This is the our full-length Practice Test . It comprises 125 multiple-choice questions covers all the domain that include Direct Patient Care , Professional Responsibilities , Safety and Infection Control , Phlebotomy and ECG/EKG with in-depth explanations.
These free Practice questions are designed to assist you in preparing for Your Patient Care Technician certification examination.
Quiz-summary
0 of 125 questions completed
Questions:
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
Information
Test Instructions
No. of Questions: 125
Questions: Multiple choice with 4 options (A, B, C, D)
Passing Score: 70% or higher
Review: You can flag questions for review and return to them
Submission: Click “Submit Test” when ready to finish
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading...
You must sign in or sign up to start the quiz.
You have to finish following quiz, to start this quiz:
Results
0 of 125 questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 points, (0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- 51
- 52
- 53
- 54
- 55
- 56
- 57
- 58
- 59
- 60
- 61
- 62
- 63
- 64
- 65
- 66
- 67
- 68
- 69
- 70
- 71
- 72
- 73
- 74
- 75
- 76
- 77
- 78
- 79
- 80
- 81
- 82
- 83
- 84
- 85
- 86
- 87
- 88
- 89
- 90
- 91
- 92
- 93
- 94
- 95
- 96
- 97
- 98
- 99
- 100
- 101
- 102
- 103
- 104
- 105
- 106
- 107
- 108
- 109
- 110
- 111
- 112
- 113
- 114
- 115
- 116
- 117
- 118
- 119
- 120
- 121
- 122
- 123
- 124
- 125
- Answered
- Review
-
Question 1 of 125
1. Question
When a patient becomes angry about their care, your most therapeutic response is:
Correct
Active listening without becoming defensive helps de-escalate situations and shows respect for patient feelings while maintaining therapeutic relationship.
Incorrect
Active listening without becoming defensive helps de-escalate situations and shows respect for patient feelings while maintaining therapeutic relationship.
-
Question 2 of 125
2. Question
Healthcare workers should receive which vaccination annually?
Correct
Annual influenza vaccination is recommended for all healthcare workers to prevent transmission to vulnerable patients and maintain workforce health.
Incorrect
Annual influenza vaccination is recommended for all healthcare workers to prevent transmission to vulnerable patients and maintain workforce health.
-
Question 3 of 125
3. Question
A patient’s pulse is weak and thready at 120 BPM. You should:
Correct
Weak, thready pulse at 120 BPM suggests possible shock, dehydration, or cardiac compromise requiring immediate nursing assessment and intervention.
Incorrect
Weak, thready pulse at 120 BPM suggests possible shock, dehydration, or cardiac compromise requiring immediate nursing assessment and intervention.
-
Question 4 of 125
4. Question
When performing capillary puncture on infant’s heel, avoid:
Correct
Central plantar area of infant heel should be avoided during capillary puncture to prevent injury to underlying bone and nerves.
Incorrect
Central plantar area of infant heel should be avoided during capillary puncture to prevent injury to underlying bone and nerves.
-
Question 5 of 125
5. Question
Lead V5 electrode is placed at:
Correct
V5 electrode placement is at left anterior axillary line in 5th intercostal space, providing lateral wall view of left ventricle.
Incorrect
V5 electrode placement is at left anterior axillary line in 5th intercostal space, providing lateral wall view of left ventricle.
-
Question 6 of 125
6. Question
A family member asks you to not tell the patient about their diagnosis. You should:
Correct
This ethical dilemma involving patient autonomy and family dynamics should be referred to the physician who can address family concerns appropriately.
Incorrect
This ethical dilemma involving patient autonomy and family dynamics should be referred to the physician who can address family concerns appropriately.
-
Question 7 of 125
7. Question
When a patient reports sudden severe headache, you should:
Correct
Sudden severe headache could indicate serious conditions like stroke, increased intracranial pressure, or hypertensive crisis requiring immediate medical evaluation.
Incorrect
Sudden severe headache could indicate serious conditions like stroke, increased intracranial pressure, or hypertensive crisis requiring immediate medical evaluation.
-
Question 8 of 125
8. Question
Used lancets should be disposed of:
Correct
Lancets are sharps that must be disposed immediately in puncture-resistant sharps containers to prevent needlestick injuries to staff.
Incorrect
Lancets are sharps that must be disposed immediately in puncture-resistant sharps containers to prevent needlestick injuries to staff.
-
Question 9 of 125
9. Question
A patient states they feel nauseous during blood draw. You should:
Correct
Nausea during blood draw may precede fainting. Stop procedure, position patient safely, and assess before continuing to prevent injury.
Incorrect
Nausea during blood draw may precede fainting. Stop procedure, position patient safely, and assess before continuing to prevent injury.
-
Question 10 of 125
10. Question
If the ECG shows ventricular rate of 180 BPM with wide QRS complexes, this suggests:
Correct
Rate of 180 BPM with wide QRS complexes indicates ventricular tachycardia, a life-threatening arrhythmia requiring immediate intervention.
Incorrect
Rate of 180 BPM with wide QRS complexes indicates ventricular tachycardia, a life-threatening arrhythmia requiring immediate intervention.
-
Question 11 of 125
11. Question
A diabetic patient’s blood glucose is 350 mg/dL. You should:
Correct
Blood glucose of 350 mg/dL indicates severe hyperglycemia possibly leading to diabetic ketoacidosis requiring immediate medical intervention.
Incorrect
Blood glucose of 350 mg/dL indicates severe hyperglycemia possibly leading to diabetic ketoacidosis requiring immediate medical intervention.
-
Question 12 of 125
12. Question
If you’re asked to perform a task you’ve never been trained for, you should:
Correct
Patient safety requires working only within your competency level. Decline tasks outside your training and request proper education first.
Incorrect
Patient safety requires working only within your competency level. Decline tasks outside your training and request proper education first.
-
Question 13 of 125
13. Question
When removing PPE, which item should be removed first?
Correct
Gloves should be removed first as they are most likely to be contaminated, preventing contamination of other PPE during removal.
Incorrect
Gloves should be removed first as they are most likely to be contaminated, preventing contamination of other PPE during removal.
-
Question 14 of 125
14. Question
When drawing blood from a patient with a fistula in their arm, you should:
Correct
Never compromise a dialysis fistula by drawing blood from that arm. Always use the opposite arm to protect the patient’s lifeline.
Incorrect
Never compromise a dialysis fistula by drawing blood from that arm. Always use the opposite arm to protect the patient’s lifeline.
-
Question 15 of 125
15. Question
A patient asks for pain medication but you’re not authorized to give it. You should:
Correct
Pain management requires nursing assessment and physician orders. Inform nurse of patient’s request for proper evaluation and treatment.
Incorrect
Pain management requires nursing assessment and physician orders. Inform nurse of patient’s request for proper evaluation and treatment.
-
Question 16 of 125
16. Question
The U wave, when present, follows the:
Correct
U waves, when visible, follow T waves and may indicate electrolyte imbalances, particularly hypokalemia requiring medical attention.
Incorrect
U waves, when visible, follow T waves and may indicate electrolyte imbalances, particularly hypokalemia requiring medical attention.
-
Question 17 of 125
17. Question
Patient confidentiality applies to:
Correct
HIPAA protects all patient health information including medical, personal, financial, and demographic data from unauthorized disclosure.
Incorrect
HIPAA protects all patient health information including medical, personal, financial, and demographic data from unauthorized disclosure.
-
Question 18 of 125
18. Question
When measuring vital signs on a patient with Parkinson’s disease, expect:
Correct
Parkinson’s disease causes tremors and movement difficulties making it challenging for patients to remain still during vital sign measurement.
Incorrect
Parkinson’s disease causes tremors and movement difficulties making it challenging for patients to remain still during vital sign measurement.
-
Question 19 of 125
19. Question
Double-bagging is required when:
Correct
Double-bagging is required when the outer bag becomes contaminated during waste removal to prevent environmental contamination.
Incorrect
Double-bagging is required when the outer bag becomes contaminated during waste removal to prevent environmental contamination.
-
Question 20 of 125
20. Question
A patient’s arm is extremely swollen. You should:
Correct
Severe swelling may indicate infection, thrombosis, or other complications. Choose alternative site and notify appropriate personnel.
Incorrect
Severe swelling may indicate infection, thrombosis, or other complications. Choose alternative site and notify appropriate personnel.
-
Question 21 of 125
21. Question
A patient on bed rest develops redness over their tailbone. This suggests:
Correct
Redness over bony prominences in immobile patients indicates Stage 1 pressure ulcer development requiring immediate intervention.
Incorrect
Redness over bony prominences in immobile patients indicates Stage 1 pressure ulcer development requiring immediate intervention.
-
Question 22 of 125
22. Question
When ECG shows peaked T waves, this may indicate:
Correct
Peaked (tall, pointed) T waves are classic sign of hyperkalemia which can cause dangerous cardiac arrhythmias requiring immediate treatment.
Incorrect
Peaked (tall, pointed) T waves are classic sign of hyperkalemia which can cause dangerous cardiac arrhythmias requiring immediate treatment.
-
Question 23 of 125
23. Question
When delegating tasks to unlicensed personnel, nurses must ensure:
Correct
Safe delegation requires ensuring the person has appropriate training, competency, and supervision to perform assigned tasks safely.
Incorrect
Safe delegation requires ensuring the person has appropriate training, competency, and supervision to perform assigned tasks safely.
-
Question 24 of 125
24. Question
Tuberculosis precautions require:
Correct
TB requires N95 respirator (properly fitted) because TB bacteria are transmitted through small airborne particles that surgical masks cannot filter.
Incorrect
TB requires N95 respirator (properly fitted) because TB bacteria are transmitted through small airborne particles that surgical masks cannot filter.
-
Question 25 of 125
25. Question
A patient complains of chest pain radiating to left arm. Priority action is:
Correct
Chest pain with radiation to left arm suggests possible myocardial infarction requiring immediate medical evaluation – time is critical.
Incorrect
Chest pain with radiation to left arm suggests possible myocardial infarction requiring immediate medical evaluation – time is critical.
-
Question 26 of 125
26. Question
When blood specimen appears milky or cloudy, this indicates:
Correct
Milky or cloudy serum/plasma indicates lipemia (high fat content) often from recent meal, which can affect certain lab test results.
Incorrect
Milky or cloudy serum/plasma indicates lipemia (high fat content) often from recent meal, which can affect certain lab test results.
-
Question 27 of 125
27. Question
The normal QT interval should be:
Correct
Normal QT interval should be less than half the R-R interval. Prolonged QT increases risk of dangerous arrhythmias like torsades de pointes.
Incorrect
Normal QT interval should be less than half the R-R interval. Prolonged QT increases risk of dangerous arrhythmias like torsades de pointes.
-
Question 28 of 125
28. Question
A coworker asks you to clock them in because they’re running late. You should:
Correct
Time clock fraud is dishonest and potentially illegal. Explain why you cannot participate in falsifying records while maintaining professional relationship.
Incorrect
Time clock fraud is dishonest and potentially illegal. Explain why you cannot participate in falsifying records while maintaining professional relationship.
-
Question 29 of 125
29. Question
When ambulating a post-operative patient for the first time, watch for:
Correct
Post-operative patients may experience orthostatic hypotension, weakness, or dizziness during first ambulation requiring careful monitoring for safety.
Incorrect
Post-operative patients may experience orthostatic hypotension, weakness, or dizziness during first ambulation requiring careful monitoring for safety.
-
Question 30 of 125
30. Question
Hand sanitizer is ineffective against which organism?
Correct
C. diff spores are resistant to alcohol-based sanitizers requiring soap and water handwashing or sporicidal disinfectants for effective removal.
Incorrect
C. diff spores are resistant to alcohol-based sanitizers requiring soap and water handwashing or sporicidal disinfectants for effective removal.
-
Question 31 of 125
31. Question
When collecting blood cultures, the number of sets typically ordered is:
Correct
Two blood culture sets from different venipuncture sites help distinguish true bacteremia from contamination during collection.
Incorrect
Two blood culture sets from different venipuncture sites help distinguish true bacteremia from contamination during collection.
-
Question 32 of 125
32. Question
A patient with swallowing difficulties should be positioned:
Correct
Patients with dysphagia should sit upright at 90 degrees during eating/drinking to use gravity and reduce aspiration risk.
Incorrect
Patients with dysphagia should sit upright at 90 degrees during eating/drinking to use gravity and reduce aspiration risk.
-
Question 33 of 125
33. Question
Artifact from patient shivering appears as:
Correct
Muscle tremor from shivering creates irregular fine artifact on ECG baseline making rhythm interpretation difficult until tremor stops.
Incorrect
Muscle tremor from shivering creates irregular fine artifact on ECG baseline making rhythm interpretation difficult until tremor stops.
-
Question 34 of 125
34. Question
Quality improvement in healthcare focuses on:
Correct
Quality improvement primarily aims to enhance patient outcomes through systematic changes in processes, safety, and care delivery.
Incorrect
Quality improvement primarily aims to enhance patient outcomes through systematic changes in processes, safety, and care delivery.
-
Question 35 of 125
35. Question
After exposure to patient’s blood, first aid includes:
Correct
Immediate washing with soap and water is first line defense after blood exposure to remove potential pathogens before other interventions.
Incorrect
Immediate washing with soap and water is first line defense after blood exposure to remove potential pathogens before other interventions.
-
Question 36 of 125
36. Question
A patient’s oxygen saturation drops to 85% during activity. You should:
Correct
Oxygen saturation of 85% during activity indicates hypoxemia requiring immediate cessation of activity and nursing assessment for intervention.
Incorrect
Oxygen saturation of 85% during activity indicates hypoxemia requiring immediate cessation of activity and nursing assessment for intervention.
-
Question 37 of 125
37. Question
Serum should be separated from cells within how many hours?
Correct
Serum should be separated from cells within 2 hours of collection to prevent cellular breakdown that could alter test results.
Incorrect
Serum should be separated from cells within 2 hours of collection to prevent cellular breakdown that could alter test results.
-
Question 38 of 125
38. Question
A heart rate of 200 BPM with narrow QRS complexes suggests:
Correct
Heart rate of 200 BPM with narrow QRS complexes indicates supraventricular tachycardia requiring immediate medical evaluation and treatment.
Incorrect
Heart rate of 200 BPM with narrow QRS complexes indicates supraventricular tachycardia requiring immediate medical evaluation and treatment.
-
Question 39 of 125
39. Question
Evidence-based practice means:
Correct
Evidence-based practice integrates current best research evidence with clinical expertise and patient preferences to guide healthcare decisions.
Incorrect
Evidence-based practice integrates current best research evidence with clinical expertise and patient preferences to guide healthcare decisions.
-
Question 40 of 125
40. Question
When a patient refuses to eat, you should:
Correct
Patient has right to refuse food. Document refusal and notify nurse so nutritional status can be assessed and alternatives considered.
Incorrect
Patient has right to refuse food. Document refusal and notify nurse so nutritional status can be assessed and alternatives considered.
-
Question 41 of 125
41. Question
Standard precautions should be used:
Correct
Standard precautions apply to all patients regardless of diagnosis treating all blood and body fluids as potentially infectious.
Incorrect
Standard precautions apply to all patients regardless of diagnosis treating all blood and body fluids as potentially infectious.
-
Question 42 of 125
42. Question
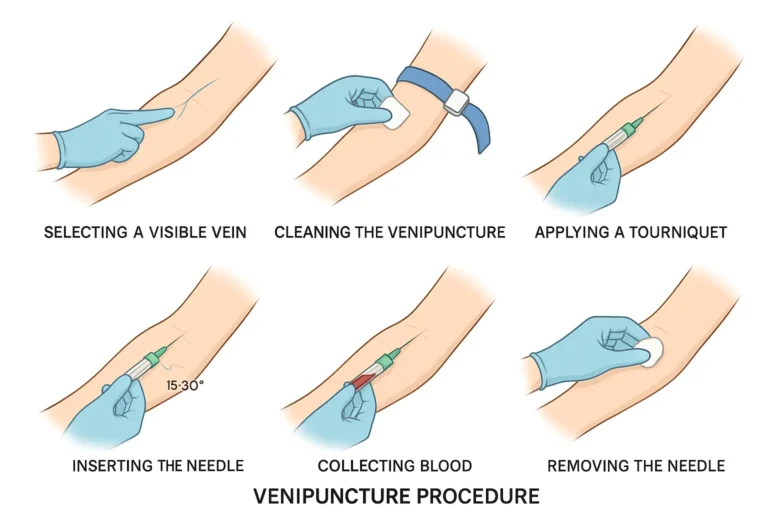
When patient has rolling veins, best technique is:
Correct
Rolling veins require firm anchoring with thumb to stabilize vein and prevent it from moving during needle insertion.
Incorrect
Rolling veins require firm anchoring with thumb to stabilize vein and prevent it from moving during needle insertion.
-
Question 43 of 125
43. Question
A confused patient keeps pulling at their IV. Best initial intervention is:
Correct
Least restrictive intervention first – use redirection and supervision before considering restraints which require physician orders.
Incorrect
Least restrictive intervention first – use redirection and supervision before considering restraints which require physician orders.
-
Question 44 of 125
44. Question
If ECG electrodes keep falling off, you should:
Correct
Electrode adhesion problems require multiple interventions: proper skin preparation, adequate gel, and firm application pressure.
Incorrect
Electrode adhesion problems require multiple interventions: proper skin preparation, adequate gel, and firm application pressure.
-
Question 45 of 125
45. Question
Mandatory reporting laws require reporting:
Correct
Healthcare workers are legally mandated to report suspected child abuse to protect vulnerable populations from harm.
Incorrect
Healthcare workers are legally mandated to report suspected child abuse to protect vulnerable populations from harm.
-
Question 46 of 125
46. Question
Proper sharps disposal requires:
Correct
Sharps must be disposed immediately after use in puncture-resistant containers without recapping to prevent needlestick injuries.
Incorrect
Sharps must be disposed immediately after use in puncture-resistant containers without recapping to prevent needlestick injuries.
-
Question 47 of 125
47. Question
A patient’s blood pressure is 210/110. Your priority is:
Correct
Blood pressure of 210/110 indicates hypertensive crisis requiring immediate medical intervention to prevent stroke or organ damage.
Incorrect
Blood pressure of 210/110 indicates hypertensive crisis requiring immediate medical intervention to prevent stroke or organ damage.
-
Question 48 of 125
48. Question
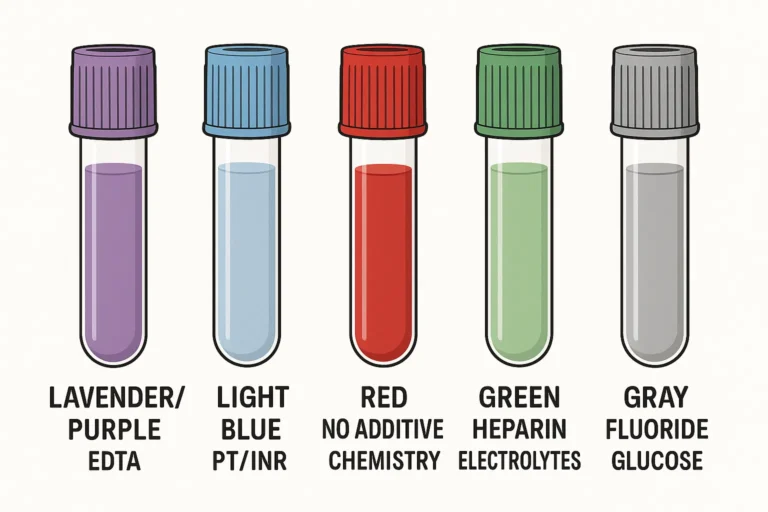
Purple top tubes should be inverted:
Correct
EDTA tubes (purple top) require 8-10 gentle inversions to properly mix anticoagulant with blood without causing hemolysis.
Incorrect
EDTA tubes (purple top) require 8-10 gentle inversions to properly mix anticoagulant with blood without causing hemolysis.
-
Question 49 of 125
49. Question
The PR interval represents:
Correct
PR interval measures time for electrical impulse to travel from SA node through AV node to begin ventricular depolarization.
Incorrect
PR interval measures time for electrical impulse to travel from SA node through AV node to begin ventricular depolarization.
-
Question 50 of 125
50. Question
Patients have the right to:
Correct
Patient autonomy includes right to refuse treatment after being informed of risks and consequences of their decision.
Incorrect
Patient autonomy includes right to refuse treatment after being informed of risks and consequences of their decision.
-
Question 51 of 125
51. Question
Contact precautions are used for:
Correct
MRSA (methicillin-resistant Staphylococcus aureus) requires contact precautions with gloves and gown to prevent transmission via direct contact.
Incorrect
MRSA (methicillin-resistant Staphylococcus aureus) requires contact precautions with gloves and gown to prevent transmission via direct contact.
-
Question 52 of 125
52. Question
When taking rectal temperature, insert thermometer:
Correct
Rectal thermometer should be inserted 1 inch in adults (1/2 inch in children) to ensure accurate reading while preventing rectal injury.
Incorrect
Rectal thermometer should be inserted 1 inch in adults (1/2 inch in children) to ensure accurate reading while preventing rectal injury.
-
Question 53 of 125
53. Question
Fasting specimens are typically collected:
Correct
Fasting specimens are typically collected in early morning after 8-12 hour overnight fast to obtain accurate baseline values.
Incorrect
Fasting specimens are typically collected in early morning after 8-12 hour overnight fast to obtain accurate baseline values.
-
Question 54 of 125
54. Question
Leads II, III, and aVF view which heart wall:
Correct
Leads II, III, and aVF are inferior leads providing view of inferior wall of left ventricle, fed by right coronary artery.
Incorrect
Leads II, III, and aVF are inferior leads providing view of inferior wall of left ventricle, fed by right coronary artery.
-
Question 55 of 125
55. Question
Informed consent must include:
Correct
Complete informed consent requires patient understanding of procedure risks, benefits, alternatives, and their right to refuse treatment.
Incorrect
Complete informed consent requires patient understanding of procedure risks, benefits, alternatives, and their right to refuse treatment.
-
Question 56 of 125
56. Question
A patient reports severe itching after medication. You should:
Correct
Severe itching after medication may indicate allergic reaction requiring immediate discontinuation and medical evaluation to prevent anaphylaxis.
Incorrect
Severe itching after medication may indicate allergic reaction requiring immediate discontinuation and medical evaluation to prevent anaphylaxis.
-
Question 57 of 125
57. Question
Airborne precautions require patient rooms to have:
Correct
Airborne precautions require negative pressure rooms that pull air in and filter it before exhaust to prevent airborne pathogens from escaping.
Incorrect
Airborne precautions require negative pressure rooms that pull air in and filter it before exhaust to prevent airborne pathogens from escaping.
-
Question 58 of 125
58. Question
When drawing blood from central line, use:
Correct
Central line blood draws require strict sterile technique including sterile gloves and maintaining sterile field to prevent line infections.
Incorrect
Central line blood draws require strict sterile technique including sterile gloves and maintaining sterile field to prevent line infections.
-
Question 59 of 125
59. Question
Normal urine output for adults is approximately:
Correct
Normal adult urine output is approximately 30-50 mL per hour (0.5-1 mL/kg/hour). Less may indicate kidney problems or dehydration.
Incorrect
Normal adult urine output is approximately 30-50 mL per hour (0.5-1 mL/kg/hour). Less may indicate kidney problems or dehydration.
-
Question 60 of 125
60. Question
Atrial fibrillation is characterized by:
Correct
Atrial fibrillation shows no clear P waves due to chaotic atrial electrical activity with irregularly irregular ventricular response.
Incorrect
Atrial fibrillation shows no clear P waves due to chaotic atrial electrical activity with irregularly irregular ventricular response.
-
Question 61 of 125
61. Question
Continuous quality improvement requires:
Correct
CQI uses systematic analysis of errors and near misses to identify system improvements that prevent future occurrences and enhance safety.
Incorrect
CQI uses systematic analysis of errors and near misses to identify system improvements that prevent future occurrences and enhance safety.
-
Question 62 of 125
62. Question
When cleaning equipment between patients, use:
Correct
Equipment cleaning between patients requires EPA-approved hospital-grade disinfectants effective against healthcare-associated pathogens.
Incorrect
Equipment cleaning between patients requires EPA-approved hospital-grade disinfectants effective against healthcare-associated pathogens.
-
Question 63 of 125
63. Question
A post-surgical patient reports pain level 9/10. Priority action is:
Correct
Severe post-operative pain (9/10) may indicate complications requiring immediate nursing assessment and pain management intervention.
Incorrect
Severe post-operative pain (9/10) may indicate complications requiring immediate nursing assessment and pain management intervention.
-
Question 64 of 125
64. Question
Therapeutic drug levels are most accurate when drawn:
Correct
Trough levels drawn just before next dose provide most accurate assessment of minimum therapeutic drug concentration.
Incorrect
Trough levels drawn just before next dose provide most accurate assessment of minimum therapeutic drug concentration.
-
Question 65 of 125
65. Question
Wide QRS complexes (>0.12 seconds) may indicate:
Correct
QRS duration >0.12 seconds indicates delayed ventricular conduction suggesting bundle branch block or ventricular arrhythmia.
Incorrect
QRS duration >0.12 seconds indicates delayed ventricular conduction suggesting bundle branch block or ventricular arrhythmia.
-
Question 66 of 125
66. Question
Patient advocacy means:
Correct
Patient advocacy involves supporting patient rights, ensuring informed decision-making, and helping navigate healthcare system complexities.
Incorrect
Patient advocacy involves supporting patient rights, ensuring informed decision-making, and helping navigate healthcare system complexities.
-
Question 67 of 125
67. Question
When measuring blood pressure, cuff should cover:
Correct
Blood pressure cuff should cover 80% of upper arm circumference for accurate readings. Wrong cuff size causes measurement errors.
Incorrect
Blood pressure cuff should cover 80% of upper arm circumference for accurate readings. Wrong cuff size causes measurement errors.
-
Question 68 of 125
68. Question
Hepatitis B vaccination provides protection for approximately:
Correct
Hepatitis B vaccination typically provides protection for 15-20 years or longer, with booster shots recommended based on antibody levels.
Incorrect
Hepatitis B vaccination typically provides protection for 15-20 years or longer, with booster shots recommended based on antibody levels.
-
Question 69 of 125
69. Question
Specimens for coagulation studies must be:
Correct
Coagulation studies require contamination-free collection with proper blood-to-anticoagulant ratio for accurate clotting time measurement.
Incorrect
Coagulation studies require contamination-free collection with proper blood-to-anticoagulant ratio for accurate clotting time measurement.
-
Question 70 of 125
70. Question
A diabetic patient appears confused and sweaty. First assessment should be:
Correct
Confusion and sweating in diabetic patient suggests possible hypoglycemia requiring immediate blood glucose assessment for appropriate intervention.
Incorrect
Confusion and sweating in diabetic patient suggests possible hypoglycemia requiring immediate blood glucose assessment for appropriate intervention.
-
Question 71 of 125
71. Question
The QT interval should be corrected for heart rate because:
Correct
QT interval naturally shortens with faster heart rates, so corrected QT (QTc) calculations adjust for rate-related changes.
Incorrect
QT interval naturally shortens with faster heart rates, so corrected QT (QTc) calculations adjust for rate-related changes.
-
Question 72 of 125
72. Question
Scope of practice violations can result in:
Correct
Working outside scope of practice can result in disciplinary action, legal liability, and harm to patients requiring various consequences.
Incorrect
Working outside scope of practice can result in disciplinary action, legal liability, and harm to patients requiring various consequences.
-
Question 73 of 125
73. Question
Eye protection is required when there is risk of:
Correct
Eye protection prevents blood and body fluid exposure to mucous membranes of eyes during procedures with splashing risk.
Incorrect
Eye protection prevents blood and body fluid exposure to mucous membranes of eyes during procedures with splashing risk.
-
Question 74 of 125
74. Question
Proper technique for using incentive spirometer is:
Correct
Incentive spirometry requires slow deep inspiration followed by 3-5 second breath hold to maximize lung expansion and prevent pneumonia.
Incorrect
Incentive spirometry requires slow deep inspiration followed by 3-5 second breath hold to maximize lung expansion and prevent pneumonia.
-
Question 75 of 125
75. Question
If blood stops flowing during venipuncture, first try:
Correct
If blood flow stops, needle may have gone through vein or against vein wall. Slightly withdrawing needle often restores flow.
Incorrect
If blood flow stops, needle may have gone through vein or against vein wall. Slightly withdrawing needle often restores flow.
-
Question 76 of 125
76. Question
Pacemaker spikes on ECG indicate:
Correct
Pacemaker spikes show electrical impulses from implanted device stimulating heart muscle when natural electrical system fails.
Incorrect
Pacemaker spikes show electrical impulses from implanted device stimulating heart muscle when natural electrical system fails.
-
Question 77 of 125
77. Question
Patient satisfaction surveys help healthcare facilities:
Correct
Patient satisfaction data helps facilities improve care quality, meet accreditation standards, and maintain competitive healthcare market position.
Incorrect
Patient satisfaction data helps facilities improve care quality, meet accreditation standards, and maintain competitive healthcare market position.
-
Question 78 of 125
78. Question
When helping patient with walker, walk:
Correct
Walk beside patient on their weaker side to provide support and assistance if they become unsteady during ambulation.
Incorrect
Walk beside patient on their weaker side to provide support and assistance if they become unsteady during ambulation.
-
Question 79 of 125
79. Question
Tuberculosis transmission occurs through:
Correct
TB spreads through small airborne droplets when infected person coughs, sneezes, or talks, requiring airborne precautions for prevention.
Incorrect
TB spreads through small airborne droplets when infected person coughs, sneezes, or talks, requiring airborne precautions for prevention.
-
Question 80 of 125
80. Question
Hemolyzed specimens are unsuitable for testing:
Correct
Hemolysis releases intracellular potassium falsely elevating serum potassium levels, making results unreliable for clinical decisions.
Incorrect
Hemolysis releases intracellular potassium falsely elevating serum potassium levels, making results unreliable for clinical decisions.
-
Question 81 of 125
81. Question
Signs of infection in surgical wound include:
Correct
Infection signs include increased warmth, redness, swelling, purulent drainage, and possibly fever requiring immediate medical attention.
Incorrect
Infection signs include increased warmth, redness, swelling, purulent drainage, and possibly fever requiring immediate medical attention.
-
Question 82 of 125
82. Question
Normal sinus rhythm requires:
Correct
Normal sinus rhythm has P wave before each QRS, rate 60-100 BPM, and regular intervals between beats.
Incorrect
Normal sinus rhythm has P wave before each QRS, rate 60-100 BPM, and regular intervals between beats.
-
Question 83 of 125
83. Question
Advance directives become effective when:
Correct
Advance directives take effect when patient loses capacity to make healthcare decisions, ensuring previously expressed wishes are followed.
Incorrect
Advance directives take effect when patient loses capacity to make healthcare decisions, ensuring previously expressed wishes are followed.
-
Question 84 of 125
84. Question
Proper technique for removing contaminated gloves:
Correct
Remove gloves by turning inside-out to contain contamination and prevent touching contaminated outer surface with bare hands.
Incorrect
Remove gloves by turning inside-out to contain contamination and prevent touching contaminated outer surface with bare hands.
-
Question 85 of 125
85. Question
A patient with heart failure should be positioned:
Correct
Heart failure patients need head elevation 30-45 degrees to reduce venous return and ease breathing by reducing pulmonary congestion.
Incorrect
Heart failure patients need head elevation 30-45 degrees to reduce venous return and ease breathing by reducing pulmonary congestion.
-
Question 86 of 125
86. Question
Butterfly needles are preferred for:
Correct
Butterfly needles provide better control for elderly patients with fragile, small, or rolling veins reducing trauma and hematoma risk.
Incorrect
Butterfly needles provide better control for elderly patients with fragile, small, or rolling veins reducing trauma and hematoma risk.
-
Question 87 of 125
87. Question
Leads V1-V6 are called:
Correct
Leads V1-V6 are precordial (chest) leads placed across chest wall providing cross-sectional view of left ventricular electrical activity.
Incorrect
Leads V1-V6 are precordial (chest) leads placed across chest wall providing cross-sectional view of left ventricular electrical activity.
-
Question 88 of 125
88. Question
Ethical principles in healthcare include:
Correct
Core ethical principles include autonomy (patient self-determination), beneficence (doing good), non-maleficence (do no harm), and justice.
Incorrect
Core ethical principles include autonomy (patient self-determination), beneficence (doing good), non-maleficence (do no harm), and justice.
-
Question 89 of 125
89. Question
Normal capillary refill time is:
Correct
Normal capillary refill should occur within 2-3 seconds after pressure release, indicating adequate peripheral circulation.
Incorrect
Normal capillary refill should occur within 2-3 seconds after pressure release, indicating adequate peripheral circulation.
-
Question 90 of 125
90. Question
Bloodborne pathogens of greatest concern include:
Correct
HIV, Hepatitis B, and Hepatitis C are primary bloodborne pathogens of concern requiring standard precautions and post-exposure protocols.
Incorrect
HIV, Hepatitis B, and Hepatitis C are primary bloodborne pathogens of concern requiring standard precautions and post-exposure protocols.
-
Question 91 of 125
91. Question
When patient has medical alert bracelet for bleeding disorder, you should:
Correct
Bleeding disorders require extended pressure application after venipuncture and careful monitoring for prolonged bleeding or hematoma formation.
Incorrect
Bleeding disorders require extended pressure application after venipuncture and careful monitoring for prolonged bleeding or hematoma formation.
-
Question 92 of 125
92. Question
A patient asks about their prognosis. You should:
Correct
Prognosis discussions involve medical judgment and should be handled by physicians who can provide accurate, comprehensive information.
Incorrect
Prognosis discussions involve medical judgment and should be handled by physicians who can provide accurate, comprehensive information.
-
Question 93 of 125
93. Question
The T wave represents:
Correct
T wave represents ventricular repolarization – the recovery phase when heart muscle resets electrically for next heartbeat.
Incorrect
T wave represents ventricular repolarization – the recovery phase when heart muscle resets electrically for next heartbeat.
-
Question 94 of 125
94. Question
Workplace violence prevention includes:
Correct
Violence prevention requires reporting threats or concerning behavior to supervisors and security for appropriate intervention and staff protection.
Incorrect
Violence prevention requires reporting threats or concerning behavior to supervisors and security for appropriate intervention and staff protection.
-
Question 95 of 125
95. Question
After accidental exposure to patient’s blood, testing may include:
Correct
Post-exposure testing typically includes baseline and follow-up testing for Hepatitis B, Hepatitis C, and HIV depending on exposure circumstances.
Incorrect
Post-exposure testing typically includes baseline and follow-up testing for Hepatitis B, Hepatitis C, and HIV depending on exposure circumstances.
-
Question 96 of 125
96. Question
When patient reports shortness of breath, priority assessment is:
Correct
Shortness of breath requires immediate oxygen saturation assessment to determine adequacy of oxygenation and need for intervention.
Incorrect
Shortness of breath requires immediate oxygen saturation assessment to determine adequacy of oxygenation and need for intervention.
-
Question 97 of 125
97. Question
Chilled specimens are required for:
Correct
Ammonia specimens must be chilled immediately and processed quickly as ammonia levels rise rapidly at room temperature affecting accuracy.
Incorrect
Ammonia specimens must be chilled immediately and processed quickly as ammonia levels rise rapidly at room temperature affecting accuracy.
-
Question 98 of 125
98. Question
If patient has chest pain during stress test, you should:
Correct
Chest pain during stress testing may indicate myocardial ischemia or infarction requiring immediate test termination and medical evaluation.
Incorrect
Chest pain during stress testing may indicate myocardial ischemia or infarction requiring immediate test termination and medical evaluation.
-
Question 99 of 125
99. Question
Continuing education helps ensure:
Correct
Continuing education maintains current knowledge and skills as healthcare practices evolve ensuring safe, effective patient care.
Incorrect
Continuing education maintains current knowledge and skills as healthcare practices evolve ensuring safe, effective patient care.
-
Question 100 of 125
100. Question
A patient’s skin feels hot and dry. This suggests:
Correct
Hot, dry skin can indicate fever, dehydration, or both conditions requiring temperature measurement and fluid status assessment.
Incorrect
Hot, dry skin can indicate fever, dehydration, or both conditions requiring temperature measurement and fluid status assessment.
-
Question 101 of 125
101. Question
Personal protective equipment should be:
Correct
PPE must be changed between patients to prevent cross-contamination and healthcare-associated infection transmission.
Incorrect
PPE must be changed between patients to prevent cross-contamination and healthcare-associated infection transmission.
-
Question 102 of 125
102. Question
When drawing multiple tubes, fill in this order:
Correct
Order of draw prevents cross-contamination between tube additives: sterile specimens first, then tubes without additives, then additive tubes.
Incorrect
Order of draw prevents cross-contamination between tube additives: sterile specimens first, then tubes without additives, then additive tubes.
-
Question 103 of 125
103. Question
Pulse deficit occurs when:
Correct
Pulse deficit exists when apical heart rate exceeds radial pulse rate, indicating some heartbeats don’t produce adequate circulation.
Incorrect
Pulse deficit exists when apical heart rate exceeds radial pulse rate, indicating some heartbeats don’t produce adequate circulation.
-
Question 104 of 125
104. Question
Artifact from 60-cycle interference appears as:
Correct
60-cycle interference from electrical equipment creates thick, fuzzy baseline artifact that can obscure cardiac rhythm interpretation.
Incorrect
60-cycle interference from electrical equipment creates thick, fuzzy baseline artifact that can obscure cardiac rhythm interpretation.
-
Question 105 of 125
105. Question
Patient care planning should be:
Correct
Patient care plans must be individualized considering patient’s unique needs, preferences, cultural factors, and medical condition.
Incorrect
Patient care plans must be individualized considering patient’s unique needs, preferences, cultural factors, and medical condition.
-
Question 106 of 125
106. Question
Needlestick injuries most commonly occur during:
Correct
Most needlestick injuries occur during needle recapping, which should be avoided by using safety devices and immediate disposal.
Incorrect
Most needlestick injuries occur during needle recapping, which should be avoided by using safety devices and immediate disposal.
-
Question 107 of 125
107. Question
When measuring temperature with temporal artery thermometer:
Correct
Temporal artery thermometers require gentle scanning motion across forehead to detect peak temperature from temporal artery.
Incorrect
Temporal artery thermometers require gentle scanning motion across forehead to detect peak temperature from temporal artery.
-
Question 108 of 125
108. Question
Clotted specimens are used for:
Correct
Clotted specimens (serum) are used for most chemistry tests after blood clots and serum is separated from cellular components.
Incorrect
Clotted specimens (serum) are used for most chemistry tests after blood clots and serum is separated from cellular components.
-
Question 109 of 125
109. Question
The ECG should be calibrated so that 1 mV equals:
Correct
Standard ECG calibration is 1 millivolt equals 10 millimeters (2 large boxes) ensuring consistent amplitude measurements across machines.
Incorrect
Standard ECG calibration is 1 millivolt equals 10 millimeters (2 large boxes) ensuring consistent amplitude measurements across machines.
-
Question 110 of 125
110. Question
Risk management focuses on:
Correct
Risk management primarily aims to identify and reduce factors that could harm patients while secondarily protecting organization from liability.
Incorrect
Risk management primarily aims to identify and reduce factors that could harm patients while secondarily protecting organization from liability.
-
Question 111 of 125
111. Question
A patient with swollen ankles should have legs:
Correct
Leg elevation above heart level uses gravity to reduce edema by promoting venous return and reducing fluid accumulation.
Incorrect
Leg elevation above heart level uses gravity to reduce edema by promoting venous return and reducing fluid accumulation.
-
Question 112 of 125
112. Question
Standard precautions include using barriers for:
Correct
Standard precautions treat all body fluids (except sweat) as potentially infectious requiring appropriate barrier protection.
Incorrect
Standard precautions treat all body fluids (except sweat) as potentially infectious requiring appropriate barrier protection.
-
Question 113 of 125
113. Question
When patient reports previous fainting during blood draw:
Correct
Patients with history of vasovagal response should lie down during blood collection to prevent injury from fainting.
Incorrect
Patients with history of vasovagal response should lie down during blood collection to prevent injury from fainting.
-
Question 114 of 125
114. Question
Orthostatic vital signs are measured:
Correct
Orthostatic vital signs measure blood pressure and pulse lying, sitting, and standing to assess for postural hypotension.
Incorrect
Orthostatic vital signs measure blood pressure and pulse lying, sitting, and standing to assess for postural hypotension.
-
Question 115 of 125
115. Question
Lead placement errors can mimic:
Correct
Incorrect lead placement can create ST changes and other artifacts that mimic myocardial infarction leading to inappropriate treatment.
Incorrect
Incorrect lead placement can create ST changes and other artifacts that mimic myocardial infarction leading to inappropriate treatment.
-
Question 116 of 125
116. Question
Incident reports should be completed:
Correct
Incident reports should be completed promptly, typically within 24 hours, while details are fresh for accurate documentation.
Incorrect
Incident reports should be completed promptly, typically within 24 hours, while details are fresh for accurate documentation.
-
Question 117 of 125
117. Question
When cleaning blood spills, work from:
Correct
Clean blood spills from center outward to prevent spreading contamination to larger areas during cleanup process.
Incorrect
Clean blood spills from center outward to prevent spreading contamination to larger areas during cleanup process.
-
Question 118 of 125
118. Question
A patient receiving diuretics should be monitored for:
Correct
Diuretics increase fluid loss requiring monitoring for dehydration, electrolyte imbalances, and kidney function changes.
Incorrect
Diuretics increase fluid loss requiring monitoring for dehydration, electrolyte imbalances, and kidney function changes.
-
Question 119 of 125
119. Question
Serum separator tubes should be:
Correct
SST tubes must clot completely (15-30 minutes) before centrifuging to ensure proper serum separation and accurate test results.
Incorrect
SST tubes must clot completely (15-30 minutes) before centrifuging to ensure proper serum separation and accurate test results.
-
Question 120 of 125
120. Question
Precordial leads V1 and V2 primarily assess:
Correct
Leads V1 and V2 are positioned over right ventricle and ventricular septum providing septal wall view of the heart.
Incorrect
Leads V1 and V2 are positioned over right ventricle and ventricular septum providing septal wall view of the heart.
-
Question 121 of 125
121. Question
Patient rights include the right to:
Correct
Patients have the right to appropriate assessment and management of pain as part of quality healthcare delivery.
Incorrect
Patients have the right to appropriate assessment and management of pain as part of quality healthcare delivery.
-
Question 122 of 125
122. Question
When assisting with deep breathing exercises, instruct patient to:
Correct
Deep breathing exercises require slow, deep inspiration through nose to maximize lung expansion and oxygenation.
Incorrect
Deep breathing exercises require slow, deep inspiration through nose to maximize lung expansion and oxygenation.
-
Question 123 of 125
123. Question
Isolation precautions are based on:
Correct
Isolation precautions are determined by how the infectious agent is transmitted (contact, droplet, airborne) rather than specific diagnosis.
Incorrect
Isolation precautions are determined by how the infectious agent is transmitted (contact, droplet, airborne) rather than specific diagnosis.
-
Question 124 of 125
124. Question
When collecting specimens for legal purposes, maintain:
Correct
Legal specimens require documented chain of custody tracking specimen handling from collection through analysis for court admissibility.
Incorrect
Legal specimens require documented chain of custody tracking specimen handling from collection through analysis for court admissibility.
-
Question 125 of 125
125. Question
The ECG rhythm strip should run for at least:
Correct
ECG rhythm strips need minimum 6 seconds (30 large boxes at 25mm/second) to adequately assess cardiac rhythm and calculate rate.
Incorrect
ECG rhythm strips need minimum 6 seconds (30 large boxes at 25mm/second) to adequately assess cardiac rhythm and calculate rate.